ALCOHOLIC LIVER DISEASE
Hello everyone.. I am varshitha , an intern posted in medicine department and one of the important terms of getting the internship completion is to complete my log book with my online log of what I learn during the course of my duties.
A 55 year old male who is a farmer by occupation came to the opd with the complaint of abdomen distension since 1 week associated with b/l pedal oedema
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 10 years back , then he noticed abdominal distension associated with b/l pedal oedema for which they went to kamineni hospital where the patient was told that he had fluid in his abdomen and it had to be removed and as told by the patient attender- the fluid was drained from the abdomen,and was put on medications for a month ( no record of medication) , he used them for a month and had relief of symptoms .During this period he had no
c/o pain abdomen , yellowish discoloration,constipation,fever, dark coloured urine
Now the patient presented to the opd (17/09/2020)with similar complaints of
abdominal distension since a week associated with b/l pedal oedema pitting type and shortness of breath
No h/o bleeding per rectum, constipation,dark coloured urine , nausea , vomitings,bleeding manifestations, blood transfusion
facial puffiness, itching, fever, involuntary movements, altered sleep wake cycle, headache, myalgia
Past History
Patient has similar complaints 10 years back ie; bilateral pedal oedema for which he got admitted in kamineni hospital and was treated for same
Personal History
Patient has a mixed diet, normal appetite with regular bowel and bladder movente, adequate sleep
He is a chronic alcoholic since 15 years , evryday he drinks 90 ml whisky , smokes 3-4 beedis evryday
Family History- not significant
General examination
Pt was conscious coherent cooperative
moderately built and nourished
Vitals - afebrile , bp- 110 /80 mmhg , pr- 86bpm rr- 16cpm
Systemic examination
P/A -
INSPECTION-
RS-
BAE present , no added sounds , trachea midline
CVS -
S1 S2 heard , no murmurs
CNS -
Higher mental functions - normal
Motor system - intact
Sensory system- intact
Cranial nerve examaination - normal
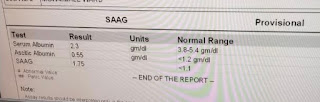
INVESTIGATIONS
Chest x ray
Patient assessed for any features of encephalopathy by doing the following psychometric tests
Treatment
- Fluid restriction upto 1.5 l/day
- salt restriction upto 2 mg/day
- syrup lactulose 15 ml/po/hs
- tab rifaximine 550 mg po bd
- tab wasilactone 20/50 mg po bd
- 3 egg whites / day
- body weight and abdominal girth monitoring
- temperature charting
Diagnosis -Alcoholic liver disease with ascitis






















Comments
Post a Comment